PSYCHOLOGY --- Depression, chapter 5 ---- Case conception in TCC and BDI
psychology·@julisavio·
0.000 HBDPSYCHOLOGY --- Depression, chapter 5 ---- Case conception in TCC and BDI
Guys, good morning. Today I will talk about a theme that is the "heart" of tcc and then I will talk about the BDI. 1- Conceptualization or case formulation 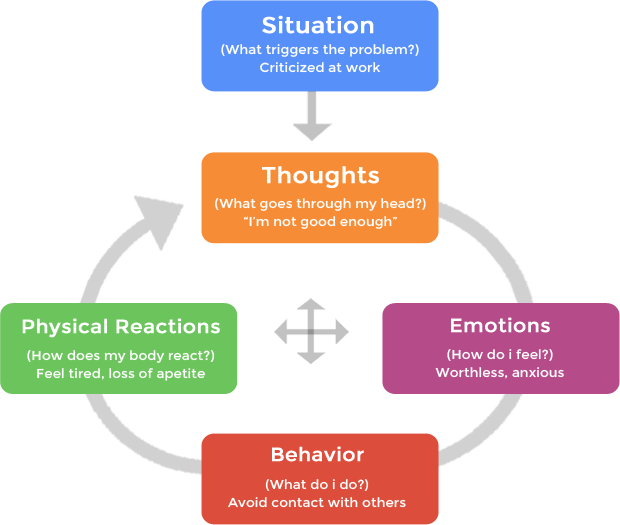 It would be a map for patient work that gathers information from seven key domains. This map is assembled by us during the first interviews. Conceptualizing within the cognitive line is fundamental to determine how the most effective course of treatment will be, since, unlike other lines, tcc is structured and focused on solving the problems presented. Usually, a session lasts 40 to 50 minutes. There is no way to know all the necessary information of the patients at that time, and a large part of them have difficulty speaking things in the first session, either because they do not understand what they present, or because they are shy when they reveal a fact of their own, because they tend to think which will be misjudged. It is made up of 7 main domains: .Diagnosis and symptoms .Factors linked to genetics and physicians .Experiences in childhood and youth that may have contributed to the patient's complaint .Affective relationship with family, friends or spouse that is influencing the situation . Strong points and qualities . Typical patterns of automatic thoughts, emotions and behaviors, for each disorder has a specific pattern of these thoughts. For example, someone with depression has poor automatic thoughts, disheartenment, despair, helplessness and always remembers their past. An anxious person tends to always think of the future and increases the problem that appears to be little in his ability to solve it. . Implicit central beliefs or beliefs. With this map drawn, we formulate our working hypothesis to assist the patient and explain to him what the treatment plan will look like, we ask for his feedback to see if he understands the proposal and accepts it. With the understanding of the plan and the proposal accepted, we begin the treatment. Always remembering that this conceptualization begins in the first contact and can be modified as the patient presents new data during the sessions, because, as previously mentioned, it is with time that rapport is created in the office (trust relationship between patient and therapist). 2- BDI ---> BECk Depression Inventory As I said in the previous post, there are some tools that help us a lot in our work, proposed by the proposer of cognitive behavioral therapy. The Beck Depression Inventory (BDI) or Beck Depression Scale was created by Aaron T. Beck. It is a questionnaire with 21 multiple choice items. It is one of the instruments most used to measure the severity of depressive episodes. the BDI is made up of 21 items referring to the person's current life that are quantified on a scale of 4 intensity points (0 to 3). The goal is to assess the intensity of depression. It is an easy questionnaire for both us and the patient. The 21 questions added up to 63 points, since each number is worth one point, for example, item 0 is worth 0 points, item 2 is worth 2 points, etc .... Zero points would be total absence of depression and 63 points would be severe depression. Nobody is in these extremes. Neither mentally healthy people have zero points nor who is depressed reaches 63. We handed the questionnaire and asked him to answer the items. He does it himself and if you have any questions ask us. It usually takes around 10 to 15 minutes to respond. If the patient takes a little longer, it may be due to lack of understanding or their depression would be "withdrawing their energy" to think and respond .... Which is more indicative. Once applied, we add up all the items and check the score. Scale scores may indicate that the person is framed within 3 levels of depression: . 10 to 18 indicates mild depression . 19 to 29 indicates moderate depression .30 to 63 indicates severe depression, of course, someone in the score of 30 is different, and another is in the range of 63. However, from 30 points, things tend to be more difficult. Usually, the use of medicines is extremely necessary here. I'll send you the BDI. I remember that it is a professional tool that only psychologists can apply. 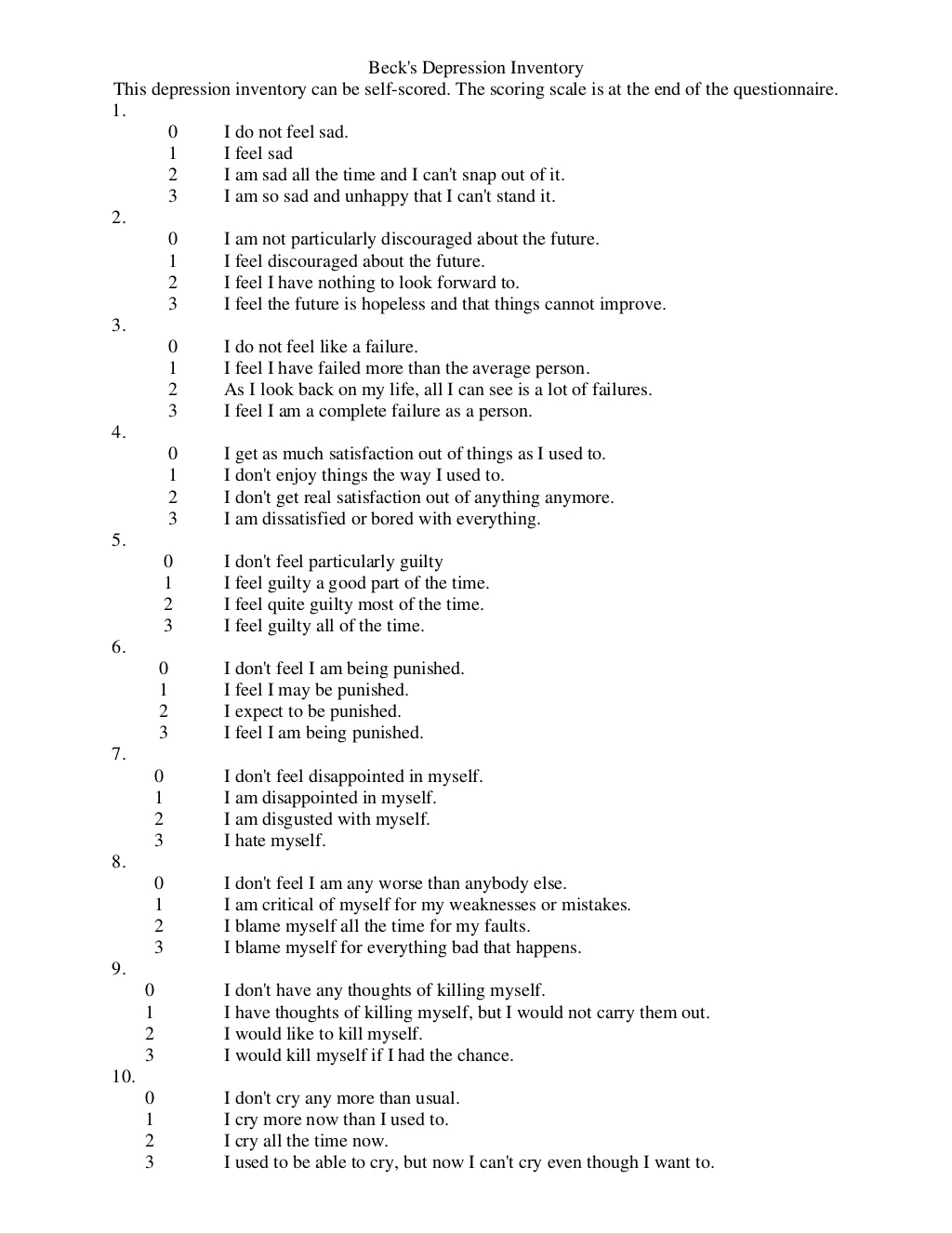 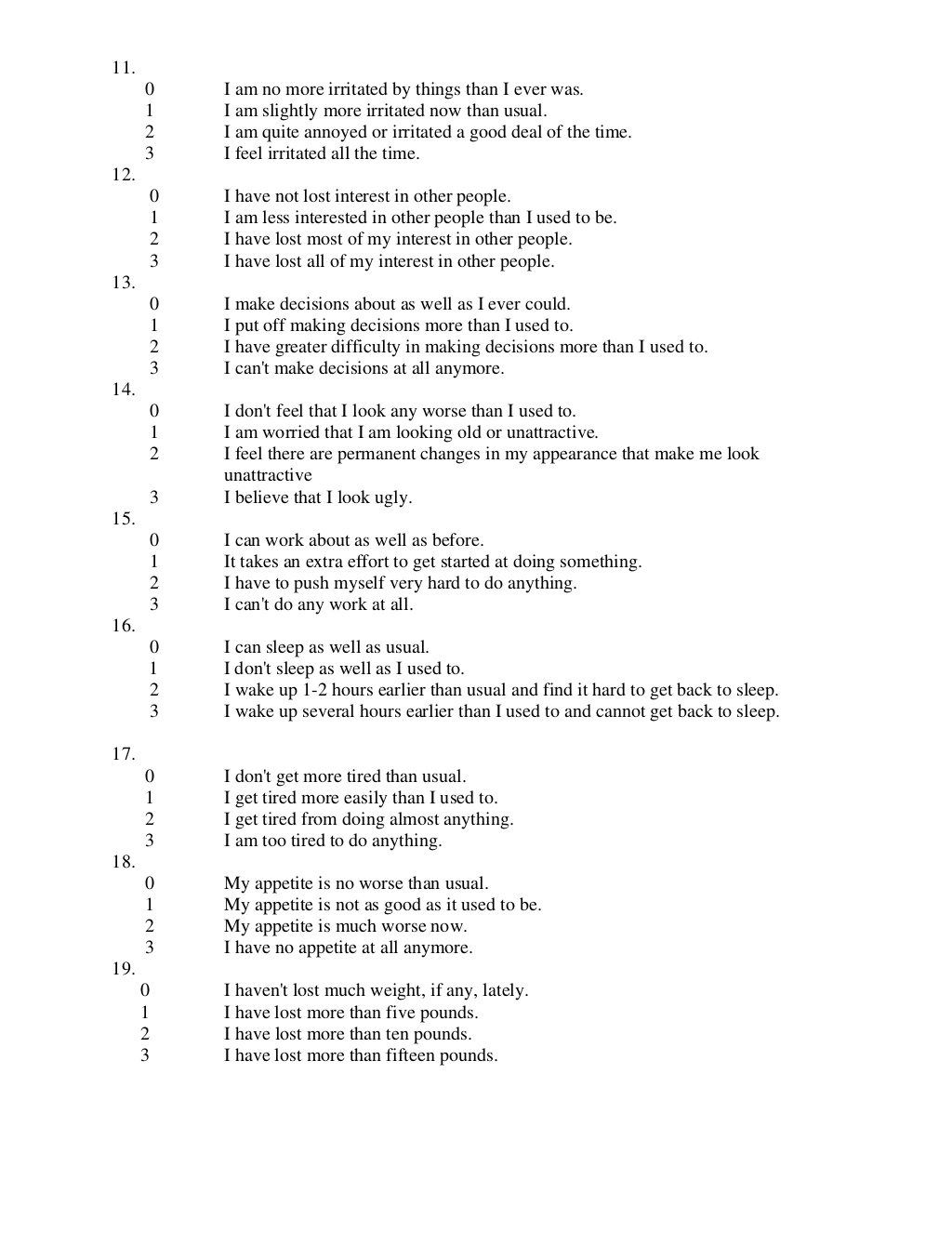 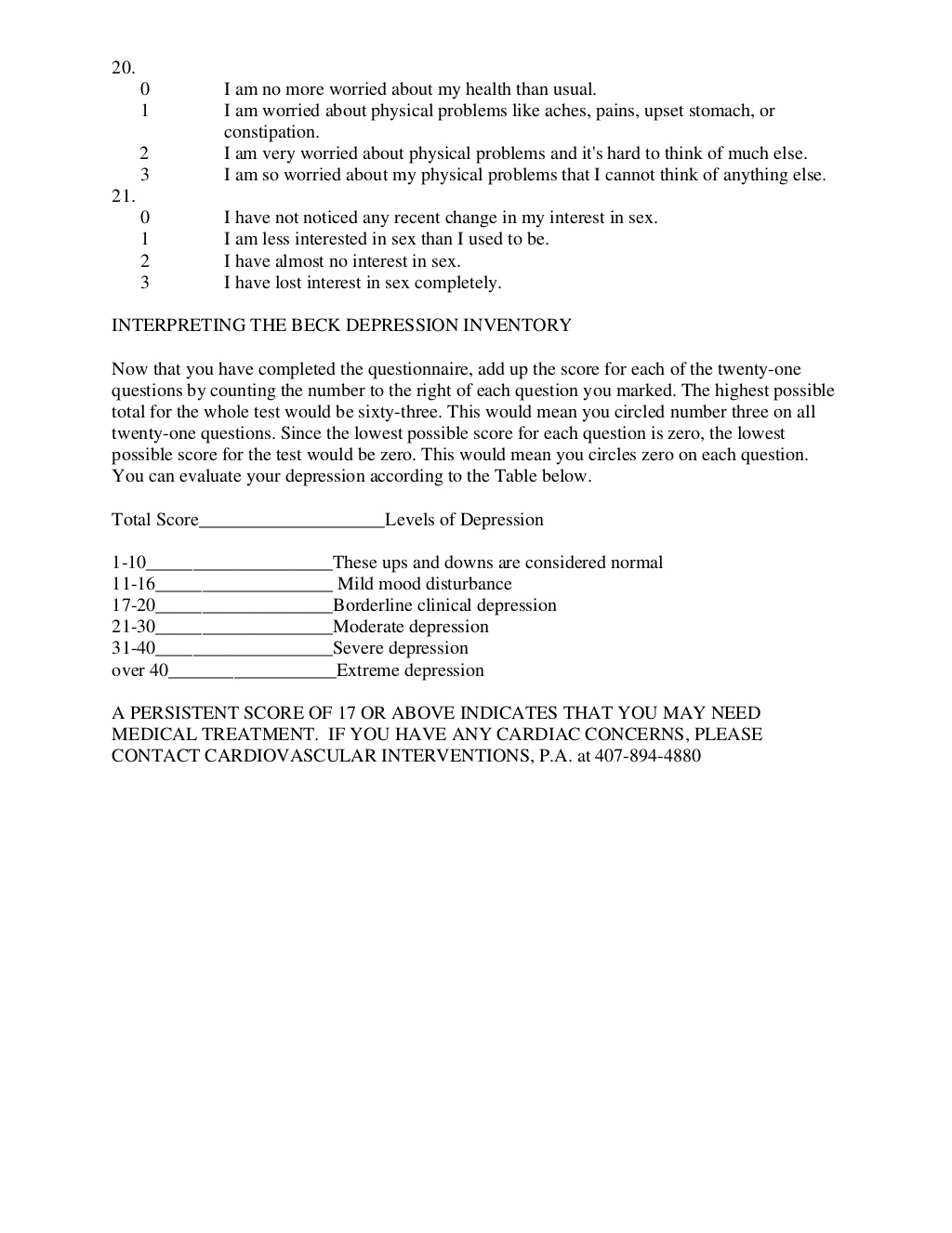 That's it people. The application of BDI helps us both to start treatment and to see how the patient's degree of depression persists during it. If the treatment is effective, the BDI score will begin to decrease, this helps us to see how the patient is progressing and whether our treatment is helping. Thank you all for reading and in the next post I will talk about the treatment of depression. If in doubt, feel free to ask in the comments. Thank you and good morning!!!